Both duodenal ulcers and benign gastric ulcers are believed to be related to mucosal infection by H.pylori.
Peptic ulcer disease are mainly classified as complicated and uncomplicated.
Benign gastric ulcer/duodenal ulcer
Age of presentation ranges from 20-60 years old, which is of course, more common among young adults.
Incidence is higher in males.
Most patients during acute presentation will present with epigastric discomfort or pain.
The intensity ranges from mild dyspepsia (related to food intake, sensation of indigestion), to severe epigastric pain, which often forces the patient to lie down still.
However, as the course of illness goes chronic, pain is rarely severe.
A characteristic feature is night pain, which is a dull, boring ache often wakes patients from sleep.
This is due to the increased gastric acidity at night, and there is lack of food to buffer against it.
The pain either radiates to the back, or towards the RHC (depends on the position of the ulcer : posterior part of stomach, duodenum)
Patient may complain of heart burn, excessive salivation (water/acid brash) related to food intake.
In duodenal ulcer, food intake relieves the symptoms. Hence, patient rarely losses appetite.
In gastric ulcer, food intake aggravates the pain and often patient is apprehensive towards food.
Hence, history of appetite and weight loss is more common in them.
Vomiting relieves the pain in gastric ulcer.
The symptoms exhibit another characteristic, which is periodicity.
As the symptoms persisted for a few weeks, then it may be followed by a period of remission for weeks to months, only to recur after that.
Hemetemesis and malena must be asked in the history as well.
History of drug intake is important, eg : NSAIDs, steroids, salicylates
Other risk factors : Period of stress, cigarette smoking
Often, in examination, apart from abdominal tenderness (guarding if severe), and pallor if there's chronic silent bleeding, there is usually no other significant findings in examination.
Investigation
Full blood count and iron studies may reveals iron deficiency anemia.
Other blood investigations - hypokalemia, increased hematocrit as a result of vomiting.
The choice of imaging in peptic ulcer disease is oesophago-gastroduodenoscopy (OGDS).
Not only it allows visualization of the lesion, it allows mucosal specimens to be biopsied.
Usually biopsy is taken from the gastric antrum, and the specimen is subjected to CLO test.
CLO test consists of inoculating the specimen into a medium containing urea.
Hence, if the specimen contains H.pylori, which produces urease.
The enzyme reacts with urea, and produces ammonia, which changes the medium from yellow to pink/red colour.
That confirms the positive status of H.pylori in the patient.
Management
Due to the finding of Peptic ulcer disease is related to H.pylori infection, the management of uncomplicated peptic ulcer disease is mainly medical.
First of all, avoid smoking, alcohol, and NSAIDs.
However, if the patient requires long courses of NSAIDs, and his/her H.pylori status is -ve, a least damaging agent should be used, such as ibuprofen.
Anti-secretory agents such as proton pump inhibitors, H2 blockers are used.
To supplement these agents, drugs like sucralfate, bismuth compounds, prostaglandin analogues are used.
Eradication of H.pylori
Regardless whether it's a duodenal ulcer/gastric ulcer, once the patient is H.pylori positive, eradication regime of H.pylori is employed.
Usually consist of 1 proton pump inhibitor and 1 or more antibiotics.
In case of duodenal ulcer, if the patient is compliant to the medication, the success rate of remission is about 90%.
Without the eradication regime, the chances of relapse within 1 year is about 80%.
Any persistence of symptoms, a urea breath test (non-invasive) should be done to reassess the H.pylori status in the patient.
However, it must be done 4 weeks after completion of the eradication regime.
Or else, the therapy merely suppresses the bacteria, and may lead to a false negative test result.
However, in gastric ulcer, biopsy need to be taken before making a diagnosis of benign gastric ulcer.
Then if found benign, eradication therapy is given to all patients with +ve status of H.pylori.
Surveillance of the lesion need to be done until the ulcer heals.
Any persistence of symptoms, further biopsy must be taken.
Perforated peptic ulcer
Occasionally, the gastric juices erodes through the gastric/duodenal wall to the extent that only covering left is the visceral peritoneum. The gastric juices collects within the peritoneal cavity, leading to chemical peritonitis.
Eventually, there'll be secondary bacterial infection, leading to spontaneous bacterial peritonitis.
History
Age of presentation : Usually 40-60 years old
History of drug intake : NSAIDs, Steroids, Salicylates
Symptoms :
Sudden onset of severe, continuous abdominal pain which initially confines to the epigastrium.
It rapidly increases in it's intensity, and eventually the pain becomes generalized.
Breathing, movements aggravates the abdominal pain.
Also ask for previous peptic ulcer disease, or history of dyspepsia.
General Examination :
Patient usually lies still on bed, breaths shallowly, and is in a state of distress.
Temperature is usually normal, there might be tachycardia.
On abdominal examination :
On inspection, the abdomen doesn't rise and fall with respiration.
This is due to the tight contraction of the abdominal musculature.
On palpation, abdominal tenderness and guarding initially confines towards the epigastrium.
Later, if the peritonitis becomes generalized, the entire abdomen is tender, and there is intense guarding.
This results in the abdomen being described of having board-like rigidity.
It is impossible to palpate for the abdominal viscus since the muscles are tightly contracted.
On percussion, there may be obliteration/diminished liver dullness (due to the air escaped from the perforated viscus into the peritoneal cavity.
Shifting dullness may be +ve.
On auscultation, bowel sound may be reduced, which indicates generalised peritonitis.
Note : 4-6 hours later, due to the dilution of the accumulated gastric juices within the peritoneal cavity, the patient's symptoms and signs subsides, and the patient actually thought that his/her condition is improving. This is mainly due to the onset of hypovolemic shock, which may be indicated by the presence of increasing abdominal distension, tachycardia, signs of dehydration and etc.
Investigation
In 60% of the patients, the CXR reveals air-filled under the diagphram.
However, absent of this finding does not exclude perforation.
Lateral Chest X-ray may be useful in case an erect CXR is not feasible (patient may be in the state of shock, disability)
In laboratory investigation, there is usually some degree of elevated serum amylase level.
However, 3-4 folds elevated serum amylase level is more suggestive of pancreatitis.
Management
1) Give fluid resuscitation
2) Analgesic for relief of pain
3) IV unasyn and flagyl
4) Anti-emetics are given
5) Insertion of NG tube, and catheterize the patient (monitoring of urine output)
Only after the patient is stable, surgical intervention is done.
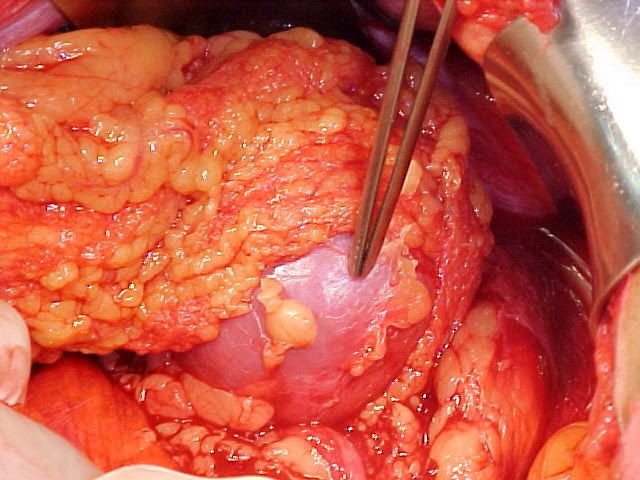
In case of a perforated duodenal ulcer, usually simple closure is performed by using an omental patch.
However, if it's a perforated gastric ulcer, a biopsy need to be taken first (to rule out malignancy)
Then, close the perforation by either simple closure or local excision.
During post-op period, IV gastric anti-secretory agent is given.
Pyloric stenosis
First of all, lets take a look at some causes of gastric outlet obstruction :
Peptic ulcer disease
Malignancy (Stomach, pancreas and lymphoma)
Crohn's disease of duodenum
Inflammation of surrounding structures
Gastroparesis (autonomic neuropathy)
Adult hypertrophic pyloric stenosis
Patients with long standing peptic ulcer disease may develop pyloric stenosis due to healing of the ulcer via fibrosis at the level of the antrum.
Usually, the complaints are :
Early satiety
Sensation of fullness, constant epigastric discomfort/pain
History of weight loss
Projectile vomiting is classical, which consists of non-bilious, undigested food particles.
It usually occurs when the patient is lying down, and following the vomiting, it relieves the sensation of fullness.
On examination, the usual findings includes :
On inspection - epigastric distension, visible peristalsis
On palpation - succussion splash ('splashing' sound heard while the abdomen is shaked right-left-right)
Investigation of choice is by OGDS, to determine the nature of obstruction (notice that the symptoms mimics malignancy)
Note that not all patients requires surgical intervention.
A course of PPI can be given first, in hope that when the ulcer heals, the stenosis is resolved.
However, if not reponsive, surgical options includes :
Pyloroplasty or Gastrojejunostomy
Gastric carcinoma
One of the most common cause of death in men.
Pernicious anemia, gastric polyps and chronic gastric ulcers are known pre-malignant conditions.
Risk factors :
1) Diet
High intake of salt, nitrosamines (usually present in preservatives)
Gastric CA is more prevalent in countries which malnutrition is a problem.
High intake of vitamin C and E seems to be protective.
2) History of surgery : Gastroenterostomy
3) Type A blood group
4) Atrophic gastritis secondary to Pernicious anemia
5) Chronic gastric ulcer
6) Gastric polyps
History
Age of onset : around 50-70 years of age
Male predominance
Any individual above 45 years of age, presenting with symptoms of dyspepsia, no matter how vague is it, should be investigated.
The epigastric discomfort may not be always associated with food intake.
Patient with long standing history of peptic ulcer disease may notice the change in the character of pain.
Usually it's the periodicity of pain becoming more constant.
There's usually complains of early satiety as well.
Another prominent symptom of Gastric CA is significant loss in appetite, which results in loss of weight.
Patient can lose around 10-20 kg of weight within 1-2 months.
If the tumour is present at the region of gastric cardia, patient may report of progressively worsening dysphagia, and eventually it may be worse enough to cause regurgitation of food contents.
If the tumour is present over the gastric outlet, there may be symptoms of gastric outlet obstruction.
Next is to sought the history of the risk factors mentioned above.
And please elicit history suggestive of metastases to the lung, liver, bones, and brain.
Examination
On general examination, the significant findings includes pallor, cachexia and probably jaundice.
Severe wasting is most noticeable over the hands and face.
Presence of jaundice (usually scleral icterus) indicates liver metastases.
Please look for evidence of an enlarged Virchow's node (left supraclavicular node)
On abdominal examination :
Inspection : abdomen is usually scaphoid, due to the severe wasting. Paradoxically, the abdomen may be distended due to malignant ascites.
Palpation : usually reveals deep tenderness over the epigastric region. In thin patients, deep palpation on full inspiration sometimes reveals a hard, irregular mass. Liver may be palpable, which is hard in consistency, knobbly in surface, non-tender.
Percussion : shifting dullness is +ve if there is malignant ascites
On systemic examination : evidence of metastases (pleural effusion, bony tenderness)







I was diagnosed with stage 3 breast cancer in August of 2010. A precious friend told me about Dr Itua Herbal Center in West Africa,She gave me his contact number and email address,I contacted him quickly so he give me guaranty that his herbal medicine will cure my cancer and i will be heal forever I said Okay.I ask him about the process for the cure,he ask me to pay for the fees which i did and within 7 working days he sent me the herbal medicine then he instructed me on how to drink it for two weeks to cure.I told Gomez my friend about the herbal medicine so he gave me go ahead to drink it.So after drinking it for two weeks i was cured I'm so grateful and i promise i will recommend anyone with cancer to him and that what i'm doing.Dr Itua Herbal Medicine makes me believes there is a hope for people suffering from,Parkinson's disease,Schizophrenia,Cancer,Scoliosis,Bladder Cancer,Colorectal Cancer,Tach Disease,Ovarian Cancer,Pancreatic Cancer,Breast Cancer,Kidney Cancer,Leukemia,Lung Cancer,Skin Cancer,
ReplyDeleteGlaucoma.measles, tetanus, whooping cough, tuberculosis, polio and diphtheria, Cataracts,Macular degeneration,Cardiovascular disease,Lung disease.Enlarged prostate,Osteoporosis.Alzheimer's disease,Obsessive Compulsive Disorder,
Dementia.Uterine Cancer,Prostate Cancer,Fibromyalgia,a
Syndrome Fibrodysplasia ,Parkinson's disease,Epilepsy Dupuytren's disease,
Diabetes ,Coeliac disease, Angiopathy, Ataxia,Arthritis,Tach Disease,Amyotrophic Lateral Sclerosis,Alzheimer's disease,Adrenocortical carcinoma.Asthma,Allergic diseases.Hiv_ Aids,Herpes,Inflammatory bowel disease ,Copd,Diabetes.
Here Is His Contact Info......[Email...drituaherbalcenter@gmail.com/ info@drituaherbalcenter.com. Whatsapp...+2348149277967]
It's a nice article. Everyone should read. For more amazing information you may get from this link
ReplyDeletepeptic ulcer